Overview
Most patients afflicted by unknown skin conditions first consult their primary care physician (PCP). Research shows that one out of ten patients presenting to a PCP has a skin condition, such as a new rash, a chronic skin condition or a changing mole as their primary chief complaint. When the PCP knows the diagnosis and treatment plan, the solution is straightforward. However, in at least 50% of cases, the etiology of the skin condition or the diagnosis of the changing mole may be unknown, resulting in the PCP seeking a dermatology referral for diagnosis or treatment. In addition to the challenges rashes present for patients, skin cancer remains the most common form of cancer in the U.S. with an estimated 1 in 5 patients developing some form of skin cancer in their lifetime. It is essential for patients to receive prompt diagnosis and appropriate triage for new skin conditions and all changing moles.
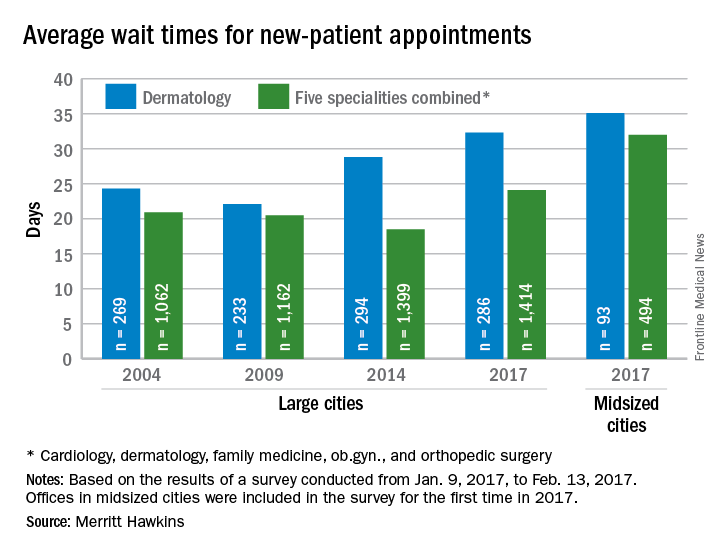
Figure 1. Average wait times in dermatology as 2017. Recent patient surveys suggest wait times upwards of 90 days for specialty appointments.
The barriers to prompt dermatologic care and treatment are many, including a lack of access to dermatological care, long delays and increased costs when available. Consequently, the wait time for dermatology referrals is long, with four in ten patients reporting a wait time of one to six months for appointments, with an additional wait time of six weeks being common for a follow-up appointment.
Figure 2. Point of care teledermatology services offers one innovative approach to helping PCPs more effectively serve their patients presenting with complex dermatological problems.
Introduction
To examine the impact of Modern Ritual Health’s novel tele-dermatology and care navigation platform, we look at a rural Family Medicine (est. 2006) clinic in North Carolina. This case study delineates the outcomes of the first four months (September - December) in its adoption of this platform, including patient and provider outcomes.
Solution Summary
In Fall of 2022, this clinic adopted the Modern Ritual Health (MRH) virtual dermatology platform. Modern Ritual dermatology is a value-based tele-dermatology, dermoscopy, and care navigation platform for primary care providers, pharmacies, urgent care, and point-of-care systems. The virtual tele-dermatology system seeks to bridge the gap between patients and the challenges in receiving prompt dermatological diagnosis and treatment for complex or unknown skin conditions.
MRH Tele-dermatology Platform Overview
- Sophisticated Hardware
- Lightweight, highly specialized tablet-compatible cameras (dermoscopes) to image moles and rashes
- Secure and Simple-to-Use Software
- Easy-to-use, five-minute process via a HIPAA-secure telehealth application
- Best-in-class dermatology provider network
- Fast, 2-day dermatology response on lesions of concern
- Care Navigation and In-person Referrals
- Care navigation, coordinating patient in-person dermatology referrals, and education
The MRH solution drastically reduces the wait time for receiving a recommendation for a lesion of concern and provides a clear outlook for future actions and treatment.
The risk assessment returns a level 1-4 based on both the severity and treatment journey for the patient’s case. Time is an especially crucial criterion for high-risk patients with a risk assessment of levels 3-4, showing a 14% decrease in overall survival rate for high risk patients treated between 30 to 59 days, decreasing further to 40% after 60 to 89 days. Therefore, reducing the time before patients have access to dermatological care is the strongest tool for recovery.
Goals & Outcomes
In this rural practice, the virtual Modern Ritual dermatology platform was used to successfully triage both lesions of concern and uncertain rashes. There are both examples of patients who were provided a piece of mind for moles that were benign, as well as serious skin lesions.
|
Benefit to Patients |
Benefit to Providers |
|
|
This process, from Modern Ritual Health alongside existing research, is shown to decrease the need for in-person patient visits by 39%.
This form of care has the potential to save $140 per newly referred dermatology patient when compared with a conventional dermatology care model . Combined with its ease of use, this platform of tele-dermatology triage provides some of the most cost-effective and significant services for detecting and diagnosing skin lesions.
Figure 2. Obtained from Modern Ritual Health de-identified data. Unnecessary referrals were reduced by about 40% in this clinics.
Level one “Normal” - These patients are most likely presenting a benign skin growth, such as a nevus.
Level two “Somewhat Abnormal” - Patients are advised to come back for a follow-up image in 3 months or at any point if they begin to notice further changes in the lesion.
Level three “Abnormal” - A level three patient is advised to receive an in-person evaluation within 4-6 weeks. In addition to text and email, a patient experience navigator may reach out to assist in referring the patient in for a faster appointment.
Level four “Very Abnormal” -
Summary
Modern Ritual offers a cost-efficient and time-saving bridge between patients and dermatological care. The services offered are crucial for getting high-risk patients the necessary care and saving time spent on unnecessary visits for low-risk patients. As such Modern Ritual teledermatology is an essential consideration for dermatological care.
Work Cited
Adam Zakaria, B. A. (2021, January 1). Cost minimization analysis of a teledermatology triage system in a managed care setting. JAMA Dermatology. Retrieved February 15, 2023, from https://jamanetwork.com/journals/jamadermatology/fullarticle/2772931
BR;, Conic RZ;Cabrera CI;Khorana AA;Gastman. “Determination of the Impact of Melanoma Surgical Timing on Survival Using the National Cancer Database.” Journal of the American Academy of Dermatology, U.S. National Library of Medicine, https://pubmed.ncbi.nlm.nih.gov/29054718/.
Delans, K., Goldstein, A. O., Goldstein, B., Grichnik, J. M., & Goldstein,, E. (n.d.). Teledermoscopy – An Emerging Technology for Skin Cancer Detection. View of teledermoscopy – an emerging technology for skin cancer detection. Retrieved February 15, 2023, from https://telehealthandmedicinetoday.com/index.php/journal/article/view/376/741
Marwaha SS;Fevrier H;Alexeeff S;Crowley E;Haiman M;Pham N;Tuerk MJ;Wukda D;Hartmann M;Herrinton LJ; (n.d.). Comparative effectiveness study of face-to-face and teledermatology workflows for diagnosing skin cancer. Journal of the American Academy of Dermatology. Retrieved February 8, 2023, from https://pubmed.ncbi.nlm.nih.gov/30738843/
“Patients Harmed by Long Waits for Dermatology Appointments, Says New Report.” Patients Harmed by Long Waits for Dermatology Appointments, Says New Report | Business Wire, 30 Apr. 2019, https://www.businesswire.com/news/home/20190430005564/en/Patients-Harmed-by-Long-Waits-for-Dermatology-Appointments-Says-New-Report.
“Skin Lesions: What They Are, Types, Causes & Treatment.” Cleveland Clinic, https://my.clevelandclinic.org/health/diseases/24296-skin-lesions.
Romaire, M. A. (2020, July). Use of primary care and specialty providers: Findings from the Medical Expenditure Panel Survey. Journal of general internal medicine. Retrieved February 15, 2023, from https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7351893/
Vaidya, T., Zubritsky, L., Alikhan, A., & Housholder, A. (2018). Socioeconomic and geographic barriers to dermatology care in urban and rural us populations. Journal of the American Academy of Dermatology, 78(2), 406–408. https://doi.org/10.1016/j.jaad.2017.07.050